As a cardiologist, I often see patients walk into my clinic with a look of pure disbelief. They are in their 30s or early 40s, lead active lives, and yet, they are facing a cardiovascular crisis. The most common phrase I hear is: “But doctor, I thought I was too young for this.”
The reality is sobering. According to recent data, heart disease remains the world’s leading cause of death, claiming nearly 20 million lives annually. What is more concerning is the rising trend of heart attacks in younger adults—those under 40.
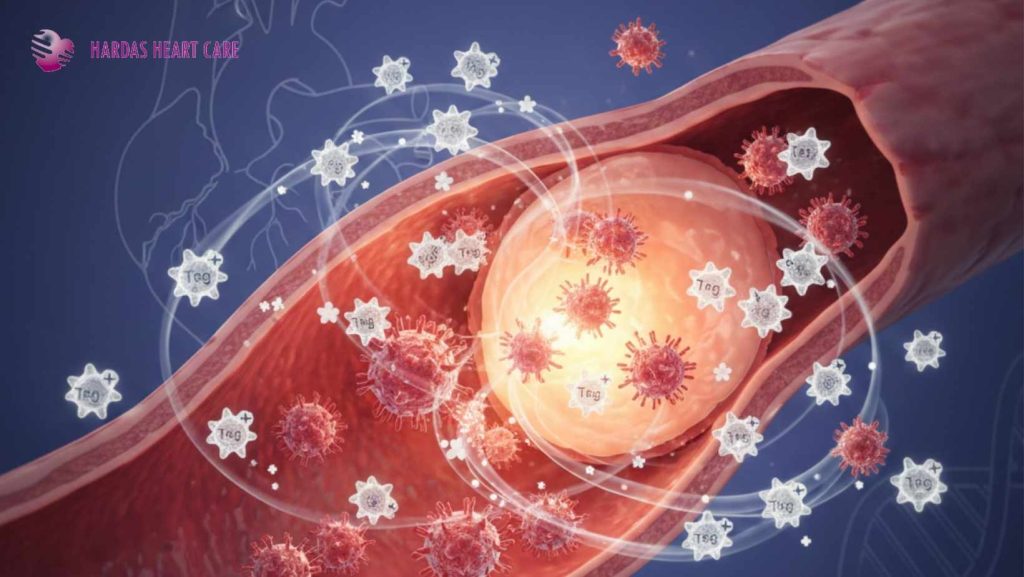
Part of why heart disease is so “sneaky” is that it often develops in silence. High blood pressure, rising glucose, and arterial inflammation don’t always cause pain until it’s too late. To protect your heart, you must first unlearn the myths that keep you from seeking care.
Here are the 12 myths I beg you to drop today.
Myth 1: “I’m too young for heart trouble.”
This is perhaps the most dangerous misconception. While risk increases with age, modern lifestyles—defined by high stress, processed foods, and sedentary habits—have pushed heart disease into the 20s and 30s. Your heart doesn’t check your ID card; it reacts to your lifestyle and genetics.
Myth 2: “If it were serious, I’d feel chest pain.”
Movies have conditioned us to look for the “Hollywood Heart Attack”—someone clutching their chest and collapsing. In reality, symptoms can be subtle: unexplained fatigue, breathlessness, jaw pain, or even persistent nausea. Women, in particular, often experience these “atypical” symptoms.
Myth 3: “I’m thin and fit, so I’m safe.”
Fitness is great, but it isn’t a suit of armor. You can look “healthy” on the outside while having high cholesterol, internal inflammation, or a genetic predisposition to heart disease. “Thin on the outside, fat on the inside” (TOFI) is a real medical concern.
Myth 4: “Exercise is dangerous once you have a heart condition.”
Many patients stop moving out of fear. While intense, unmonitored workouts can be risky, guided and moderate exercise is actually a cornerstone of cardiac recovery. It strengthens the heart muscle and improves circulation.
Myth 5: “My family has heart issues, so my fate is sealed.”
Genetics load the gun, but lifestyle pulls the trigger. Even with a strong family history, you can significantly delay or prevent heart disease through regular screenings, stress management, and a heart-healthy diet.
Myth 6: “Women don’t need to worry as much as men.”
This is a fatal misunderstanding. Heart disease is a leading killer of women globally. Because symptoms in women are often ignored or misdiagnosed as anxiety or indigestion, they frequently arrive at the hospital later than men.
Myth 7: “Once I have a procedure, I’m cured.”
A stent or a bypass is a “mechanical fix,” not a permanent cure. It opens the road, but it doesn’t stop the “rust” (plaque) from forming elsewhere. Post-procedure care, medication, and lifestyle changes are lifelong commitments.
Myth 8: “My cholesterol is normal, so my heart is fine.”
Cholesterol is just one piece of the puzzle. We also look at blood pressure, blood sugar, inflammation markers (like CRP), and lifestyle factors. You can have “perfect” cholesterol and still be at high risk due to stress or smoking.
Myth 9: “I’ll be stuck on heart medication forever.”
Not necessarily. While some medications are protective for the long term, dosages can often be adjusted or even reduced if a patient makes significant, sustained lifestyle improvements. However, never stop medication without a doctor’s guidance.
Myth 10: “If I feel fine, nothing is wrong.”
Conditions like hypertension (high blood pressure) are called “silent killers” for a reason. You can feel perfectly energetic while your arteries are under immense pressure. Regular check-ups catch what your “feelings” cannot.
Myth 11: “I exercise, so I can eat whatever I want.”
You cannot outrun a bad diet. High salt, processed sugars, and trans fats cause damage to the lining of your arteries that a 30-minute jog cannot simply “erase.” Heart health is built in the kitchen as much as in the gym.
Myth 12: “I’ll start worrying about my heart when I’m 50.”
The foundation for a heart attack at 50 is often laid in your 20s. Prevention is a lifelong journey. By the time symptoms appear, the disease is usually advanced.
The Bottom Line
Only about 35% of people go for preventive heart check-ups; the rest only show up after a crisis. Don’t wait for the “Golden Hour”—the first hour after a heart attack where treatment is most effective. Act now by scheduling a screening.
Your heart works every second of your life. It’s time you started listening to what it’s trying to tell you.